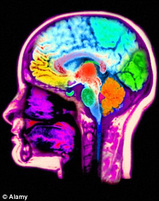
 Neuroscientists claim to have found a way to predict whether convicted criminals are likely to re-offend by looking at their brain scans According to American imaging experts, convicts showing low activity in an area of the brain associated with decision-making and action are more likely to be arrested again. A team led by Kent Kiehl, a neuroscientist at the Mind Research Network in Albuquerque, studied a group of 96 male prisoners shortly before they were due to be released. READ MORE http://www.dailymail.co.uk/sciencetech/article-2299423/Brain-scans-predict-criminal-likely-reoffend.html Dr. Pry and Congressman Roscoe Bartlett: Dr. Peter Pry, formerly a CIA analyst and staff to Congressman Bartlett and the EMP Commission he helped launch, reviewed the history of those trying to address this issue beginning with the formation of the EMP Commission to current day attempts at legislation to address the issues. He introduced Congressman Roscoe Bartlett who noted that just as people think some things are "just too good to be true", that similarly, "other things are just too bad to be true" claiming that EMP and these high-impact threats are examples of the latter. Congressman Bartlett's long-term history of wrestling with high-impact threats to infrastructure such as the electric power grids parallels his long standing congressional leadership in energy security and the role of renewable energy. Congressman Bartlett reviewed the history of his involvement of both high-impact threats to critical infrastructure with special emphasis on manmade EMP and space weather along with his related interest in energy security. He answered audience questions and led questioning of other presenters throughout the morning session. For more information on InfraGard and its national EMP SIG, see InfraGard.net. Bioterrorism and the Pandemic Potential March 7, 2013 | 1001 GMT Print 20 17 48 9 Text Size Stratfor By Rebecca Keller Periodic media reports of bird flu, a new SARS-like virus and a case of drug-resistant tuberculosis have kept the world informed, but they have also contributed to a distorted perception of the true threat such contagions pose. Perhaps the greatest value of the media coverage is the opportunity it provides to discuss the uncertainties and the best ways to prepare for biological threats, both natural and man-made. It is important to remember that the risk of biological attack is very low and that, partly because viruses can mutate easily, the potential for natural outbreaks is unpredictable. The key is having the right tools in case of an outbreak, epidemic or pandemic, and these include a plan for containment, open channels of communication, scientific research and knowledge sharing. In most cases involving a potential pathogen, the news can appear far worse than the actual threat. Infectious Disease Propagation Since the beginning of February there have been occurrences of H5N1 (bird flu) in Cambodia, H1N1 (swine flu) in India and a new, or novel, coronavirus (a member of the same virus family as SARS) in the United Kingdom. In the past week, a man from Nepal traveled through several countries and eventually ended up in the United States, where it was discovered he had a drug-resistant form of tuberculosis, and the Centers for Disease Control and Prevention released a report stating that antibiotic-resistant infections in hospitals are on the rise. In addition, the United States is experiencing a worse-than-normal flu season, bringing more attention to the influenza virus and other infectious diseases. The potential for a disease to spread is measured by its effective reproduction number, or R-value, a numerical score that indicates whether a disease will propagate or die out. When the disease first occurs and no preventive measures are in place, the reproductive potential of the disease is referred to as R0, the basic reproduction rate. The numerical value is the number of cases a single case can cause on average during its infectious period. An R0 above 1 means the disease will likely spread (many influenza viruses have an R0 between 2 and 3, while measles had an R0 value of between 12 and 18), while an R-value of less than 1 indicates a disease will likely die out. Factors contributing to the spread of the disease include the length of time people are contagious, how mobile they are when they are contagious, how the disease spreads (through the air or bodily fluids) and how susceptible the population is. The initial R0, which assumes no inherent immunity, can be decreased through control measures that bring the value either near or below 1, stopping the further spread of the disease. Both the coronavirus family and the influenza virus are RNA viruses, meaning they replicate using only RNA (which can be thought of as a single-stranded version of DNA, the more commonly known double helix containing genetic makeup). The rapid RNA replication used by many viruses is very susceptible to mutations, which are simply errors in the replication process. Some mutations can alter the behavior of a virus, including the severity of infection and how the virus is transmitted. The combination of two different strains of a virus, through a process known as antigenic shift, can result in what is essentially a new virus. Influenza, because it infects multiple species, is the hallmark example of this kind of evolution. Mutations can make the virus unfamiliar to the body's immune system. The lack of established immunity within a population enables a disease to spread more rapidly because the population is less equipped to battle the disease. The trajectory of a mutated virus (or any other infectious disease) can reach three basic levels of magnitude. An outbreak is a small, localized occurrence of a pathogen. An epidemic indicates a more widespread infection that is still regional, while a pandemic indicates that the disease has spread to a global level. Virologists are able to track mutations by deciphering the genetic sequence of new infections. It is this technology that helped scientists to determine last year that a smattering of respiratory infections discovered in the Middle East was actually a novel coronavirus. And it is possible that through a series of mutations a virus like H5N1 could change in such a way to become easily transmitted between humans. Lessons Learned There have been several influenza pandemics throughout history. The 1918 Spanish Flu pandemic is often cited as a worst-case scenario, since it infected between 20 and 40 percent of the world's population, killing roughly 2 percent of those infected. In more recent history, smaller incidents, including an epidemic of the SARS virus in 2003 and what was technically defined as a pandemic of the swine flu (H1N1) in 2009, caused fear of another pandemic like the 1918 occurrence. The spread of these two diseases was contained before reaching catastrophic levels, although the economic impact from fear of the diseases reached beyond the infected areas. Previous pandemics have underscored the importance of preparation, which is essential to effective disease management. The World Health Organization lays out a set of guidelines for pandemic prevention and containment. The general principles of preparedness include stockpiling vaccines, which is done by both the United States and the European Union (although the possibility exists that the vaccines may not be effective against a new virus). In the event of an outbreak, the guidelines call for developed nations to share vaccines with developing nations. Containment strategies beyond vaccines include quarantine of exposed individuals, limited travel and additional screenings at places where the virus could easily spread, such as airports. Further measures include the closing of businesses, schools and borders. Individual measures can also be taken to guard against infection. These involve general hygienic measures -- avoiding mass gatherings, thoroughly washing hands and even wearing masks in specific, high-risk situations. However, airborne viruses such as influenza are still the most difficult to contain because of the method of transmission. Diseases like noroviruses, HIV or cholera are more serious but have to be transmitted by blood, other bodily fluids or fecal matter. The threat of a rapid pandemic is thereby slowed because it is easier to identify potential contaminates and either avoid or sterilize them. Research is another important aspect of overall preparedness. Knowledge gained from studying the viruses and the ready availability of information can be instrumental in tracking diseases. For example, the genomic sequence of the novel coronavirus was made available, helping scientists and doctors in different countries to readily identify the infection in limited cases and implement quarantine procedures as necessary. There have been only 13 documented cases of the novel coronavirus, so much is unknown regarding the disease. Recent cases in the United Kingdom indicate possible human-to-human transmission. Further sharing of information relating to the novel coronavirus can aid in both treatment and containment. Ongoing research into viruses can also help make future vaccines more efficient against possible mutations, though this type of research is not without controversy. A case in point is research on the H5N1 virus. H5N1 first appeared in humans in 1997. Of the more than 600 cases that have appeared since then, more than half have resulted in death. However, the virus is not easily transmitted because it must cross from bird to human. Human-to-human transmission of H5N1 is very rare, with only a few suspected incidents in the known history of the disease. While there is an H5N1 vaccine, it is possible that a new variation of the vaccine would be needed were the virus to mutate into a form that was transmittable between humans. Vaccines can take months or even years to develop, but preliminary research on the virus, before an outbreak, can help speed up development. In December 2011, two separate research labs, one in the United States and one in the Netherlands, sought to publish their research on the H5N1 virus. Over the course of their research, these labs had created mutations in the virus that allowed for airborne transmission between ferrets. These mutations also caused other changes, including a decrease in the virus's lethality and robustness (the ability to survive outside the carrier). Publication of the research was delayed due to concerns that the results could increase the risk of accidental release of the virus by encouraging further research, or that the information could be used by terrorist organizations to conduct a biological attack. Eventually, publication of papers by both labs was allowed. However, the scientific community imposed a voluntary moratorium in order to allow the community and regulatory bodies to determine the best practices moving forward. This voluntary ban was lifted for much of the world on Jan. 24, 2013. On Feb. 21, the National Institutes of Health in the United States issued proposed guidelines for federally funded labs working with H5N1. Once standards are set, decisions will likely be made on a case-by-case basis to allow research to continue. Fear of a pandemic resulting from research on H5N1 continues even after the moratorium was lifted. Opponents of the research cite the possibility that the virus will be accidentally released or intentionally used as a bioweapon, since information in scientific publications would be considered readily available. The Risk-Reward Equation The risk of an accidental release of H5N1 is similar to that of other infectious pathogens currently being studied. Proper safety standards are key, of course, and experts in the field have had a year to determine the best way to proceed, balancing safety and research benefits. Previous work with the virus was conducted at biosafety level three out of four, which requires researchers wearing respirators and disposable gowns to work in pairs in a negative pressure environment. While many of these labs are part of universities, access is controlled either through keyed entry or even palm scanners. There are roughly 40 labs that submitted to the voluntary ban. Those wishing to resume work after the ban was lifted must comply with guidelines requiring strict national oversight and close communication and collaboration with national authorities. The risk of release either through accident or theft cannot be completely eliminated, but given the established parameters the risk is minimal. The use of the pathogen as a biological weapon requires an assessment of whether a non-state actor would have the capabilities to isolate the virulent strain, then weaponize and distribute it. Stratfor has long held the position that while terrorist organizations may have rudimentary capabilities regarding biological weapons, the likelihood of a successful attack is very low. Given that the laboratory version of H5N1 -- or any influenza virus, for that matter -- is a contagious pathogen, there would be two possible modes that a non-state actor would have to instigate an attack. The virus could be refined and then aerosolized and released into a populated area, or an individual could be infected with the virus and sent to freely circulate within a population. There are severe constraints that make success using either of these methods unlikely. The technology needed to refine and aerosolize a pathogen for a biological attack is beyond the capability of most non-state actors. Even if they were able to develop a weapon, other factors such as wind patterns and humidity can render an attack ineffective. Using a human carrier is a less expensive method, but it requires that the biological agent be a contagion. Additionally, in order to infect the large number of people necessary to start an outbreak, the infected carrier must be mobile while contagious, something that is doubtful with a serious disease like small pox. The carrier also cannot be visibly ill because that would limit the necessary human contact. As far as continued research is concerned, there is a risk-reward equation to consider. The threat of a terrorist attack using biological weapons is very low. And while it is impossible to predict viral outbreaks, it is important to be able to recognize a new strain of virus that could result in an epidemic or even a pandemic, enabling countries to respond more effectively. All of this hinges on the level of preparedness of developed nations and their ability to rapidly exchange information, conduct research and promote individual awareness of the threat. Read more: Bioterrorism and the Pandemic Potential | Stratfor |
AuthorPreska Thomas Archives
June 2013
Categories |

 RSS Feed
RSS Feed